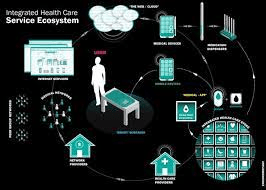
How are hospitals and health systems positioning their organizations for the future in a post-pandemic world? While there are countless ways innovation has accelerated the transformation of healthcare delivery over the past year, here are six worth noting:
- Artificial intelligence
- Cloud technology
- Virtual ICU
- Collaboration
- Inpatient telehealth through specially equipped in-room televisions
- Virtual Reality
HealthLeaders has spoken to innovators at multiple organizations who share their insights with our readers. These are their stories:
1. ARTIFICIAL INTELLIGENCE: 5 CONSIDERATIONS FOR HEALTH SYSTEMS
Artificial intelligence (AI) holds tremendous potential to change dynamics in healthcare, but it is also one of the least understood technologies, as myths, promises, and valid concerns create confusion in the landscape. Regardless, AI is a fast-growing technology sector, predicted to reach $6.6 billion this year by consulting firm Accenture, which also forecasts that key clinical health AI applications could potentially create $150 billion in annual savings for the U.S. healthcare economy by 2026.
To gain further insight into the concerns and opportunities hospitals and health systems face, HealthLeaders spoke to experts Children’s Health, OSF HealthCare, and Dallas-based Pieces, which spun out of the non-profit research institute Parkland Center for Clinical Innovation (PCCI), an organization affiliated with Parkland Health & Hospital System.
2. MAYO CLINIC AND GOOGLE TAKE RELATIONSHIP TO NEXT LEVEL
In a move that further cements the growing relationship between Mayo Clinic and Google, the Mountain View, California-based tech firm announced it is opening a permanent office in Mayo Clinic’s hometown of Rochester, Minnesota. Collaboration to transform patient care has already resulted in enhanced radiotherapy delivery processes, development of an AI factory, and moving 10 million patient records to the cloud.
Since forging a partnership in 2019, “We’ve been hard at work laying the technical groundwork for a lot of innovation, with security and privacy foundational to everything we do,” said Cris Ross, MBA, chief information officer, Mayo Clinic, during a press briefing on Thursday. “Having this new space to facilitate our collaboration will really help us accelerate innovation and work towards a shared vision of a data-centric future, which we think can transform patient, care, and provider experiences and reduce the cost of care.”
3. 5 LESSONS AHN LEARNED WHILE LAUNCHING A VIRTUAL ICU DURING THE PANDEMIC
In a quest to build a virtual ICU program for multiple hospitals in its 13-hospital health system, Allegheny Health Network (AHN), Pittsburgh-based Highmark Health not only boosted its capacity to care for critically ill patients, it also built the infrastructure for expansion of future virtual care initiatives.
“As we think about the broader scope of where virtual care can go, the virtual ICU becomes a microcosm of how you can begin to expand it because you have that kind of scalability,” says Anil Singh, MD, MPH, MMM, executive medical director, enterprise clinical organization-clinical solutions, design, and implementation, Highmark Health.
While AHN will use this foundation to explore other virtual initiatives, Highmark plans to work with other local provider partners and AHN to execute similar strategies in local markets.
4. HOW COLLABORATION ACCELERATES INNOVATION DURING THE PANDEMIC
During the pandemic, the symbiotic relationship between health systems and the vendors that serve them has intensified, resulting in close collaborations to adapt existing products to meet emerging needs. The relationship between Phoenix-based Banner Health, which operates 29 hospitals in six states, and Boston-based Kyruus expanded to meet emerging needs to address COVID-19 testing and vaccination scheduling.
Representatives from both organizations worked together to adapt the product, and Top of FormBottom of Formthe benefits now extended far beyond Banner’s service area. The vaccine scheduling enhancement is now being used by 14 other health systems.
“It’s a virtuous cycle of continuous improvement and continually using creativity to take existing technologies, repurpose them, and use them in more meaningful ways that truly transform your business,” says Christen Castellano, vice president of customer experience channels, Banner Health.
5. TELEHEALTH TVS POSITION INTERMOUNTAIN FOR THE FUTURE OF VIRTUAL CARE
Intermountain Healthcare has outfitted smart televisions in patient rooms with devices from Amwell that transform the TV set into a telehealth portal, replete with a pan, tilt, and zoom camera and special microphone. With the ability to add third parties to the conversation and screen sharing capabilities, the system creates efficiencies, enhances collaboration, and positions the health system for the next phase of virtual care.
The initiative is so promising, “We’re embedding the infrastructure for telehealth into all of our architectural plans,” says Brian Wayling, MBA, assistant vice president of telehealth services, Intermountain Healthcare.
6. 5 WAYS VIRTUAL REALITY CAN BETTER PREPARE FUTURE SURGEONS
With elective surgeries halted or postponed during the past year, the coronavirus pandemic could have yet another unanticipated impact on the future of healthcare by delaying training for surgical residents.
To address this issue, a virtual reality (VR) training program used by the orthopaedic surgery residency program at Marshall University Joan C. Edwards School of Medicine suddenly has gained more relevance. The way Marshall is using VR today shines a light on some inherent challenges with surgical training and how this evolving technology could prepare a new generation of surgeons for the increasingly complex repertoire of procedures they are now expected to perform.
Blog Credits Earned to Mandy Roth (Health Leaders)